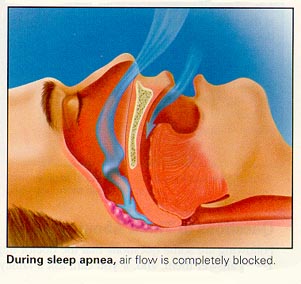
Acupuncture Treatment is to use needles to stimulate acupoints along meridians to invigorate energy and blood circulation. Most cases of sleep apnea are caused by the collapse of soft tissue around the throat where the air passing is blocked. Enlarged tongue or low muscle tone protrude towards the back of throat making air difficult to pass.
Dr. Wang has successfully treated many patients with his special technique. During the treatment, he selects particular points that improve circulation and mucosal immunity so to reduce the resistance and that help increase tongue muscle tone. The space between the tongue and the back wall of throat is thus enlarged and maintained.
Patients usually have better sleep, less apnea events and feel better during the day after a few treatments. In order to get long term effect, regular treatments are needed. The effective is almost 100%, that means all the patients have seen improvement. Long term benifit is to reduce the risk of heart, lung complications and maintain sugar and cholesterol level within normal range.
Sleep apnea is a sleep disorder characterized by abnormal pauses in breathing or instances of abnormally low breathing, during sleep. Each pause in breathing, called an apnoea, can last from a few seconds to minutes, and may occur 5 to 30 times or more an hour. Similarly, each abnormally low breathing event is called a hypopnea. Sleep apnoea is diagnosed with an overnight sleep test called apolysomnogram, or a "sleep study".
There are three forms of sleep apnoea: central (CSA), obstructive (OSA), and complex or mixed sleep apnoea (i.e., a combination of central and obstructive) constituting 0.4%, 84% and 15% of cases respectively. In CSA, breathing is interrupted by a lack of respiratory effort; in OSA, breathing is interrupted by a physical block to airflow despite respiratory effort and snoring is common.
Regardless of type, an individual with sleep apnoea is rarely aware of having difficulty breathing, even upon awakening. Sleep apnoea is recognized as a problem by others witnessing the individual during episodes or is suspected because of its effects on the body . Symptoms may be present for years (or even decades) without identification, during which time the sufferer may become conditioned to the daytime sleepiness and fatigue associated with significant levels of sleep disturbance.
Obstructive sleep apnea is the most common category of sleep-disordered breathing. The muscle tone of the body ordinarily relaxes during sleep, and at the level of the throat the human airway is composed of collapsible walls of soft tissue which can obstruct the breathing during sleep. Mild occasional sleep apnea, such as many people experience during an upper respiratory infection, may not be important, but chronic severe obstructive sleep apnea requires treatment to prevent low blood oxygen (hypoxemia), sleep deprivation, and other complications. The most serious complication is a severe form of congestive heart failure called cor pulmonale.
Individuals with low muscle tone and soft tissue around the airway (e.g., because of obesity) and structural features that give rise to a narrowed airway are at high risk for obstructive sleep apnea. The elderly are more likely to have OSA than young people. Men are more likely to suffer sleep apnea than women and children are, though it is not uncommon in the latter two population groups.
The risk of OSA rises with increasing body weight, active smoking and age. In addition, patients with diabetes or "borderline" diabetes have up to three times the risk of having OSA.
Common symptoms include loud snoring, restless sleep, and sleepiness during the daytime. Diagnostic tests include home oximetry or polysomnography in a sleep clinic.
Some treatments involve lifestyle changes, such as avoiding alcohol or muscle relaxants, losing weight, and quitting smoking. Many people benefit from sleeping at a 30-degree elevation of the upper body or higher, as if in a recliner. Doing so helps prevent the gravitational collapse of the airway. Lateral positions(sleeping on a side), as opposed to supine positions (sleeping on the back), are also recommended as a treatment for sleep apnea, largely because the gravitational component is smaller in the lateral position. Some people benefit from various kinds of oral appliances to keep the airway open during sleep. "Breathing machines" like the continuous positive airway pressure (CPAP) may help. There are also surgical procedures to remove and tighten tissue and widen the airway.
As already mentioned, snoring is a common finding in people with this syndrome. Snoring is the turbulent sound of air moving through the back of the mouth, nose, and throat. Although not everyone who snores is experiencing difficulty breathing, snoring in combination with other conditions such as overweight and obesity has been found to be highly predictive of OSA risk. The loudness of the snoring is not indicative of the severity of obstruction, however. If the upper airways are tremendously obstructed, there may not be enough air movement to make much sound. Even the loudest snoring does not mean that an individual has sleep apnea syndrome. The sign that is most suggestive of sleep apneas occurs when snoring stops. If both snoring and breathing stop while the person's chest and body try to breathe, that is literally a description of an event in obstructive sleep apnea syndrome. When breathing starts again, there is typically a deep gasp and then the resumption of snoring.
Other indicators include (but are not limited to): hypersomnolence, obesity BMI >30, large neck circumference (16 in (410 mm) in women, 17 in (430 mm) in men), enlarged tonsils and large tongue volume, micrognathia, morning headaches, irritability/mood-swings/depression, learning and/or memory difficulties, and sexual dysfunction.
The term "sleep-disordered breathing" is commonly used in the U.S. to describe the full range of breathing problems during sleep in which not enough air reaches the lungs (hypopnea and apnea). Sleep-disordered breathing is associated with an increased risk of cardiovascular disease, stroke, high blood pressure, arrhythmias, diabetes, and sleep deprived driving accidents. When high blood pressure is caused by OSA, it is distinctive in that, unlike most cases of high blood pressure (so-called essential hypertension), the readings do not drop significantly when the individual is sleeping. Stroke is associated with obstructive sleep apnea. Sleep apnea sufferers also have a 30% higher risk of heart attack or premature death than those unaffected.
In the June 27, 2008, edition of the journal Neuroscience Letters, researchers revealed that people with OSA show tissue loss in brain regions that help store memory, thus linking OSA with memory loss. Using magnetic resonance imaging (MRI), the scientists discovered that sleep apnea patients' mammillary bodies were nearly 20 percent smaller, particularly on the left side. One of the key investigators hypothesized that repeated drops in oxygen lead to the brain injury.
Treatment
For mild cases of sleep apnea, a treatment which is a lifestyle change is sleeping on one's side, which can prevent the tongue and palate from falling backwards in the throat and blocking the airway. Another is avoiding alcohol and sleeping pills, which can relax throat muscles, contributing to the collapse of the airway at night.
For moderate to severe sleep apnea, the most common treatment is the use of a continuous positive airway pressure (CPAP) device, which 'splints' the patient's airway open during sleep by means of a flow of pressurized air into the throat. The patient typically wears a plastic facial mask, which is connected by a flexible tube to a small bedside CPAP machine. The CPAP machine generates the required air pressure to keep the patient's airways open during sleep. Advanced models may warm or humidify the air and monitor the patient's breathing to insure proper treatment. Although CPAP therapy is extremely effective in reducing apneas and less expensive than other treatments, some patients find it extremely uncomfortable. Many patients refuse to continue the therapy or fail to use their CPAP machines on a nightly basis. The CPAP machine assists only inhaling, whereas a BiPAP machine assists with both inhaling and exhaling and is used in more severe cases.
In addition to CPAP, dentists specializing in sleep disorders can prescribe Oral Appliance Therapy (OAT). The oral appliance is a custom-made mouthpiece that shifts the lower jaw forward, opening up the airway. OAT is usually successful in patients with mild to moderate obstructive sleep apnea. OAT is a relatively new treatment option for sleep apnea in the United States, but it is much more common in Canada and Europe. Its use has led to increasing recognition of the importance of upper airway anatomy in the pathophysiology of OSA.
CPAP and OAT are generally effective only for obstructive and mixed sleep apnea which have a mechanical rather than a neurological cause.
For patients who do not tolerate or fail nonsurgical measures, surgical treatment to anatomically alter the airway is available. Several levels of obstruction may be addressed, including the nasal passage, throat (pharynx), base of tongue, and facial skeleton. Surgical treatment for obstructive sleep apnea needs to be individualized in order to address all anatomical areas of obstruction. Often, correction of the nasal passages needs to be performed in addition to correction of the oropharynx passage. Septoplasty and turbinate surgery may improve the nasal airway. Tonsillectomy and uvulopalatopharyngoplasty (UPPP or UP3) is available to address pharyngeal obstruction. Base-of-tongue advancement by means of advancing the genial tubercle of the mandible may help with the lower pharynx. A myriad of other techniques are available, including hyoid bone myotomy and suspension and various radiofrequency technologies. For patients who fail these operations, the facial skeletal may be advanced by means of a technique called maxillomandibular advancement, or two-jaw surgery (upper and lower jaws). Technically, this is accomplished by a surgery similar to orthognathic surgeries addressing an abnormal bite. The surgery involves a Lefort type one osteotomy and bilateral sagittal split mandibular osteotomies
Other surgery options may attempt to shrink or stiffen excess tissue in the mouth or throat, procedures done at either a doctor's office or a hospital. Small shots or other treatments, sometimes in a series, are used for shrinkage, while the insertion of a small piece of stiff plastic is used in the case of surgery whose goal is to stiffen tissues.[21]
Possibly owing to changes in pulmonary oxygen stores, sleeping on one's side (as opposed to on one's back) has been found to be helpful for central sleep apnea with Cheyne-Stokes respiration (CSA-CSR).
Medications like Acetazolamide lower blood pH and encourage respiration. Low doses of oxygen are also used as a treatment for hypoxia but are discouraged due to side effects.
Surgery
CPAP is the most consistently safe and effective treatment for obstructive sleep apnea but it is not a cure, and people are less likely to use it in the long term. In contrast, although not well known, surgery is more expensive and can treat directly the causes of sleep apnea: The Stanford Center for Excellence in Sleep Disorders Medicine achieved a 95% cure rate of sleep apnea patients by surgery. Maxillomandibular advancement (MMA) is considered the most effective surgery for sleep apnea patients because it increases the posterior airway space (PAS). The main benefit of the operation is that the oxygen saturation in the arterial blood increases. In a study published in 2008, 93.3.% of surgery patients achieved an adequate quality of life based on the Functional Outcomes of Sleep Questionnaire (FOSQ). Surgery led to a significant increase in general productivity, social outcome, activity level, vigilance, intimacy and sex, and the total score postoperatively was P = .0002. Overall risks of MMA surgery are low: The Stanford University Sleep Disorders Center found 4 failures in a series of 177 patients, or about one out of 44 patients.
Several inpatient and outpatient procedures use sedation. Many drugs and agents used during surgery to relieve pain and to depress consciousness remain in the body at low amounts for hours or even days afterwards. In an individual with either central, obstructive or mixed sleep apnea, these low doses may be enough to cause life-threatening irregularities in breathing or collapses in a patient¨s airways. Use of analgesics and sedatives in these patients postoperatively should therefore be minimized or avoided.
Surgery on the mouth and throat, as well as dental surgery and procedures, can result in postoperative swelling of the lining of the mouth and other areas that affect the airway. Even when the surgical procedure is designed to improve the airway, such as tonsillectomy and adenoidectomy or tongue reduction, swelling may negate some of the effects in the immediate postoperative period. Once the swelling resolves and the palate becomes tightened by postoperative scarring, however, the full benefit of the surgery may be noticed. Individuals with sleep apnea generally require more intensive monitoring after surgery for these reasons.
Sleep apnea patients undergoing any medical treatment must make sure his or her doctor and/or anesthetist are informed about their condition. Alternate and emergency procedures may be necessary to maintain the airway of sleep apnea patients. If an individual suspects he or she may have sleep apnea, communication with their doctor about possible preprocedure screening may be in order.